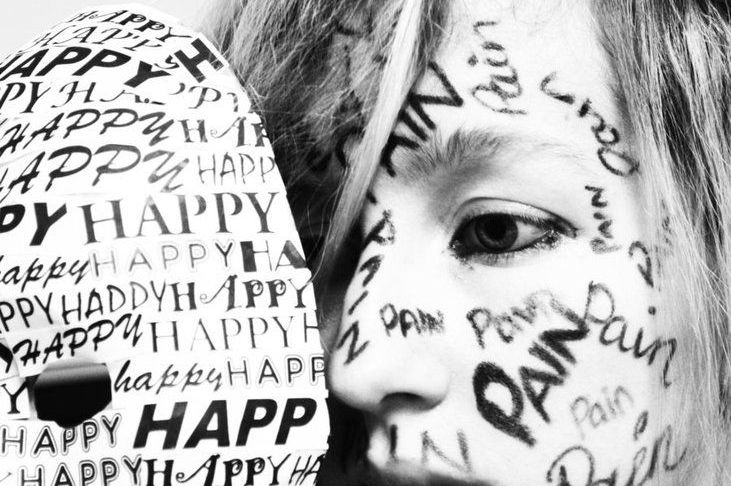
Obsessive compulsive disorder (OCD) is a psychiatric disorder characterized by recurrent thoughts, accompanied by completely irrational and unmotivated fears and worries, that lead the sufferer to continuously repeat, in an obsessive and uncontrolled manner, certain actions or processes in an attempt to appease anxiety and protect himself from nefarious events otherwise deemed inevitable, despite the fact that they are, in reality, highly unlikely.
Disorders and symptoms
Often, the activities performed by OCD sufferers are completely “normal” and harmless, but they become pathological because of the obsession with which they are repeated and the inability to do without them. Typical compulsive behaviors include: obsessive and repeated washing of hands, hair, or the entire body, in fear of contamination; the verification, repeated even dozens of times, of having closed the gas or windows before leaving the house; the arrangement of clothes, objects, books in a definite and unchangeable order.
Not infrequently, those suffering from obsessive compulsive disorder nag friends and family members (often the mother) with continuous and exasperating requests for reassurance that he is combed, that he has no blemishes or marks on his skin, that his teeth are clean, or that he is being helped to “better check” details that cause agitation and anxiety and that he fears he cannot sufficiently check for himself.
If
obsessive compulsive disorder
is not treated, over time, obsessive-compulsive behaviors multiply and worsen, leading to serious deterioration of quality of life and family relationships, social and work withdrawal, with disabling outcomes. In addition, medical problems related to the effects of obsessive behaviors (such as dermatitis or alopecia due to excessive washing) and suicidal thoughts may ensue. To prevent these unfavorable developments, it is crucial that the affected person’s family members seek medical advice from the earliest signs of illness, turning first to the family physician or directly to the psychiatrist.
Causes
The causes of obsessive compulsive disorder are not known, but the disease is believed to be driven by a complex interaction between predisposing genetic factors (yet to be determined) and exposure to stressful stimuli or events during childhood or later stages of life, as well as possible specific environmental factors (e.g., infections), but these remain to be specified and verified.
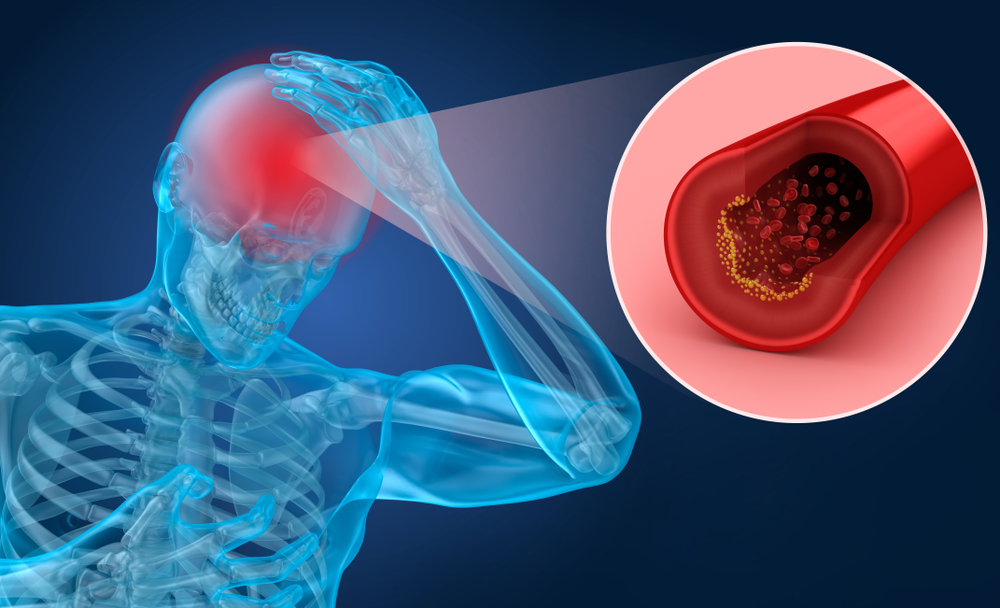
You are more likely to be affected by the disease if you also suffer from other psychiatric disorders (in particular, pertaining to the area of anxiety disorders and the depression), if one has predisposing personality traits (perfectionism, excessive tendency to apprehension and control, insecurity, etc.), and if other people in the family suffer from obsessive compulsive disorder (in particular, one or both parents). Neurologically, obsessive compulsive disorder is linked to a series of alterations in the functioning of brain circuits that regulate impulsivity, emotions, and stress response, to date, only partially characterized.
Diagnosis
The diagnosis of obsessive compulsive disorder is based on the finding of various types of behaviors and actions characterized by obsessive repetition, compulsion, and an inability to give up performing them without going through severe and disabling anxiety and distress. Sometimes, recognizing the disease is not easy because the manifestations may be partly overlapping with those of other psychiatric disorders such as anxiety, forms of depression with psychotic features, or schizophrenia. The diagnosis of obsessive compulsive disorder is, in many cases, delayed because the sufferer’s family members tend to become accustomed to the extravagant behaviors and underestimate the severity of the warning signs, even adopting, more or less consciously, a “protective” attitude or denial of the illness.
The diagnostic delay also depends on the fact that, often, the patient’s family members also exhibit personality traits similar to those typical of obsessive compulsive disorder, albeit at a subclinical level, and thus have less “sensitivity” in recognizing the disease. In the case of recent onset of obsessive-compulsive manifestations, especially in people without a family history of the disease, possible specific triggers should be investigated, such as the presence of organic diseases (e.g., thyroid disorders) or the taking of drugs (in particular, dopamine agonists, used to treat Parkinson’s disease) or substances of abuse (alcohol, psychostimulants, etc.).
How to treat
The therapeutic interventions needed to regress obsessive compulsive disorder should be identified according to the severity of the manifestations, the patient’s age, and the duration of the illness. If the disorder has arisen recently and/or is not particularly severe, the first proposed approach is psycho-behavioral and is aimed at achieving progressive “deconditioning” from obsessive-compulsive habits, starting with those that create milder discomfort and interfere less with daily activities. In essence, you try to “dishabituate” the patient to perform the established rituals and make them feel less and less necessary.
When the disorder is more invasive and/or has been present for a long time, it becomes necessary to add drug therapy to psychotherapeutic interventions in order to achieve appreciable clinical outcomes. The drugs of choice for the treatment of obsessive compulsive disorder are antidepressants, particularly those belonging to the serotonin-releasing system inhibitor (SSRI) and norepinephrine-releasing system inhibitor (SNRI) classes, which should be taken for several months, continuing for some time even after the symptoms have disappeared.
Depending on the characteristics of the disorder in the individual patient, in some cases, it may be necessary to combine antidepressants with drugs of a different type, such as antipsychotics. In selected patients inadequately controlled by psychotherapy and drug treatments, deep brain stimulation may be considered (Deep Brain Stimulation
, DBS), involving implantation of microelectrodes that are designed to stimulate specific brain circuits involved in impulse control.