Follow a healthy, balanced diet, moving every day and taking prescribed therapies regularly is the key to keeping diabetes under control and preventing complications associated with advanced stages of the disease, especially affecting the cardiovascular system (atherosclerosis and acute events, such as heart attack and stroke), kidneys (diabetic nephropathy), eyes (diabetic macular degeneration) and peripheral nerves (diabetic neuropathy).
A recent Italian study, conducted in collaboration between a research team from the Institute of Cell Biology and Neurobiology of the National Research Council (IBCN-CNR), the IRCCS Fondazione Santa Lucia in Rome, the University of Chieti and the University of Milan, now reports that eating less could also have more specific positive implications on the last mentioned issue.
What is diabetic neuropathy
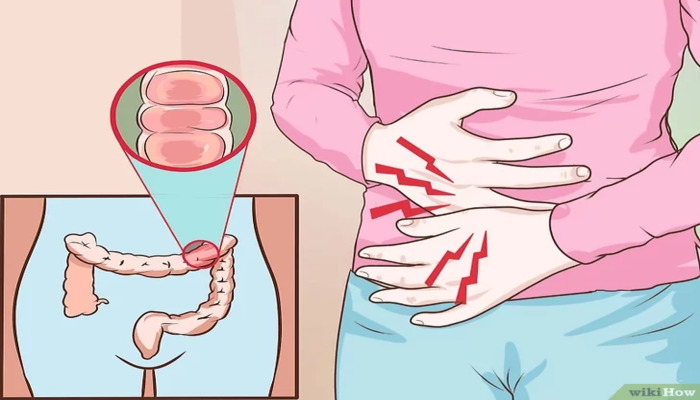
Diabetic neuropathy is one of the most dreaded complications of diabetes, both type 1 and type 2, responsible for the onset of tingling, loss or alteration of sensation, and intense pain that is difficult to control with common analgesics, mainly in the hands, feet, arms, and legs.
Neuropathy is, moreover, a co-factor in the origin of“diabetic foot” (still the leading nontraumatic cause of amputation), since the reduced skin sensitivity it brings about prevents detection of small, accidental wounds that can quickly become infected and induce extensive necrosis, which is difficult to manage and regress.
The origin of neuropathy is complex and not yet fully elucidated, but it is well established that inadequate blood glucose control for prolonged periods (evidenced by glycated hemoglobin, HbA1c, values in the blood above 6.0-6.5%) and increased general inflammatory state of the body are key pathogenic elements of sensitization and degeneration of peripheral nerve endings.
Why the low-calorie diet helps
Numerous studies have shown that cutting dietary calorie intake not only helps reduce body weight, prevent type 2 diabetes and help control blood sugar, but also increases metabolic efficiency and decreases the degree of systemic inflammation. Building on these considerations, IBCN-CNR researchers tested the effects of a restrictive diet, maintained for short periods of time, on the state and repair process of peripheral nerves in mice.
“In our experiments, we found that after peripheral sciatic nerve damage, a dietary regimen with reduced daily caloric intake acts as a powerful metabolic stimulus and activator of a fundamental cell survival and turnover mechanism known as autophagy (the cell incorporates damaged parts of itself).”, explained Sara Marinelli of IBCN-CNR, coordinator of the project.
The researchers also showed the same recovery from neuropathic pain in animals showing low cell renewal capacity. “These animals with reduced autophagy capacity have underlying diabetic-like metabolic alterations that aggravate the neuropathy condition,” pointed out Roberto Coccurello of IBCN-CNR. “Well, even with these complications, restricting calorie intake can counteract the course and intensity of neuropathic pain by restoring a metabolic balance, reducing inflammatory processes, and facilitating nerve regeneration through stimulation of autophagy. All this, in the absence of manifest side effects, as is the case with continued use of the pharmacological approach alone.”.
Although obtained in animal models and yet to be verified in humans, the new evidence paves the way for innovative therapeutic strategies that have been awaited for years. In addition, through this study the researchers were able to identify some early biological markers of neurological damage that could be very useful in clinical practice to assess the prognosis of neuropathy in the individual patient and, therefore, to plan more effective personalized treatments.
Source:
Coccurello R et al. Effects of caloric restriction on neuropathic pain, peripheral nerve degeneration and inflammation in normometabolic and autophagy-deficient prediabetic Ambra1 mice. PlosOne 2018;13(12):e0208596. doi:10.1371/journal.pone.0208596