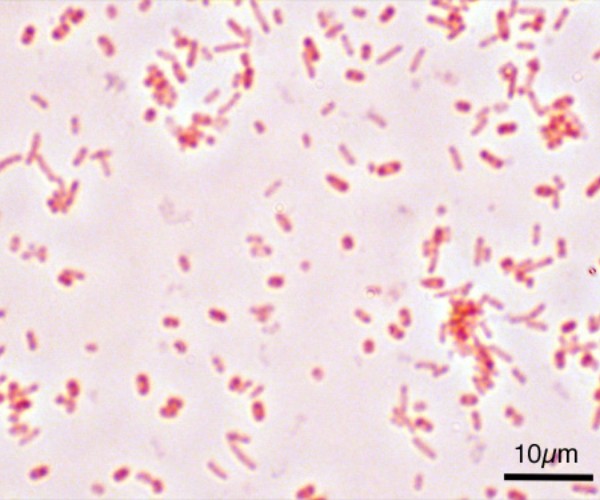
The microbial structure in the intestine is greatly influenced by the type of power type, and it of its own goes on to influence a number of metabolic, hormonal and neurological processes, based on a study of available work performed by scholars at George Washington University (GW) and the National Institute of Standards and Technology (NIST). The article was later published in Nutrition Reviews. The human microbiome has until recently been an under-examined topic to seek new strategies for disease diagnosis and treatment. At present, the number of those diseases that can result in disruption of the gut microbiome seems to be increasing and prevailing, and the scientific community is not aligned on a consensus of what can define a microbiome as a “healthy gut.” The GW and NIST review systematically made assessments of current thinking on existing interactions between nutrition and the gut microbiome in healthy adults. Leigh A. Frame, PhD, MHS, director of the integrative medicine program at the GW School of Medicine and Health Sciences said “As we learn more about the gut microbiome and nutrition, we also learn how influential they are on each other and what role they both play in disease prevention and treatment, a topic very central to public health“.
Through their review of the papers, the authors inferred that the relationship in the two directions between nutrition and the intestinal microbiome is emerging , while more research is being conducted on the process by which the microbiota utilizes and produces both macro- and micronutrients. The authors found that the research focused primarily on the benefits of dietary fiber, which serves as fuel for the gut microbiota, and also observing that protein promotes the metabolism of “microbial proteins” and potentially harmful byproducts that can remain in the gut, causing an increased risk of adverse health outcomes.”This observation reveals that the current measurement tools we possess are ineffective in identifying microbial and molecular hallmarks that can serve as valid indicators of health and disease” said Scott Jackson, adjunct assistant professor of clinical research and leadership at SMHS and leader of SMHS, NIST’s Complex Microbial Systems Group.
The authors suggest that future research should consider individual responses to different diets and how the gut microbiome responds to them, but also the emphasized function of the microbiome.
Source: International Research