The pancreas plays an important role in the digestion of food. Pancreatic diseases, both acute and chronic, can create inevitable problems in both dietetics and artificial nutrition. The exocrine pancreas secretes between 1500 and 3000 mL/day of alkaline pH fluid containing at least 20 enzymes that are the main component of digestion. This function is regulated by the autonomic nervous system, entero-hormones, insulin and bile salts.
Pancreatitis acute
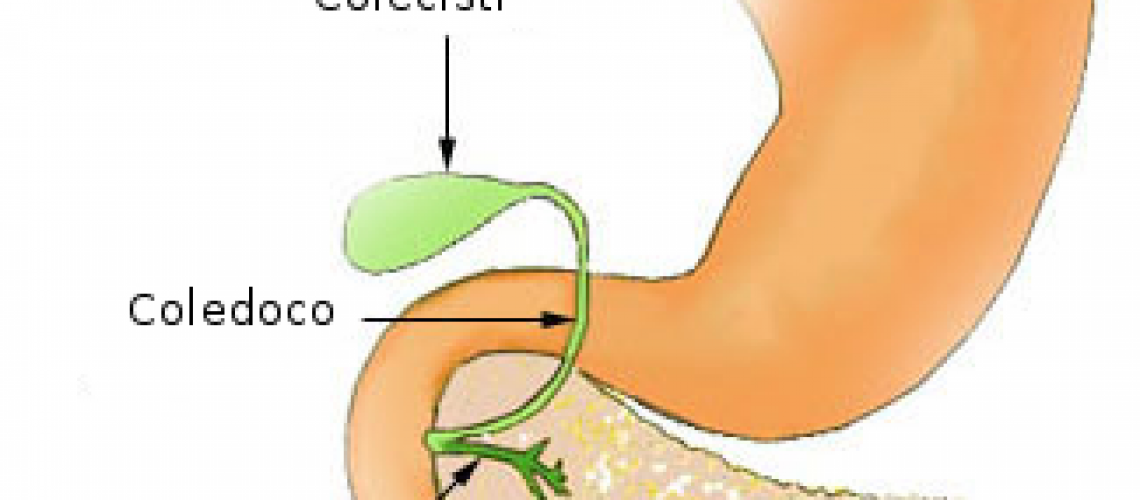
There are many causes of this condition, but the most common are cholecystic stones, alcoholism, and hypertriglyceridemia. Acute pancreatitis in most cases is a reversible condition that does not bring pathological effects to the pancreatic organ. The clinical-nutritional intervention includes an initial period of parenteral nutrition aimed at hydro-electrolyte rebalancing and containment of protein catabolism. Subsequently, enteral nutrition can be envisaged, using naso-digiunal tube and complete os supplements and then semi-liquid feeding.
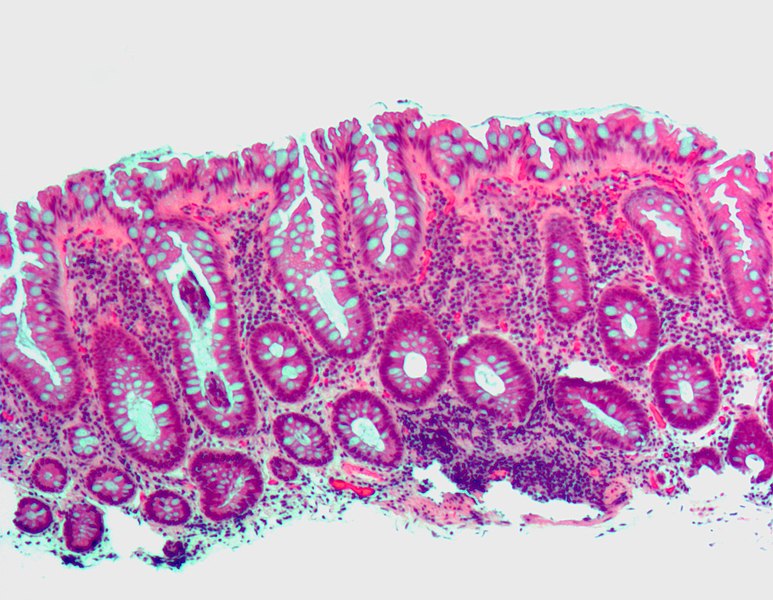
Pancreatitis chronic
In This case involves permanently irreversible damage to the pancreas, characterized by abdominal pain, diabetes mellitus, and steatorrhea. The causes main are related to abnormal feeding habits. Symptomatology that conditions reduced food intake is represented by pain abdominal and from various digestive disorders. The regular use of Pancreatic enzyme preparations leads to an improvement in the steatorrhea. The goal in this form of pancreatitis is to prevent the establishment of Of malnutrition.
Source: Handbook of Dietetics and Clinical Nutrition by Franco Contaldo et al.