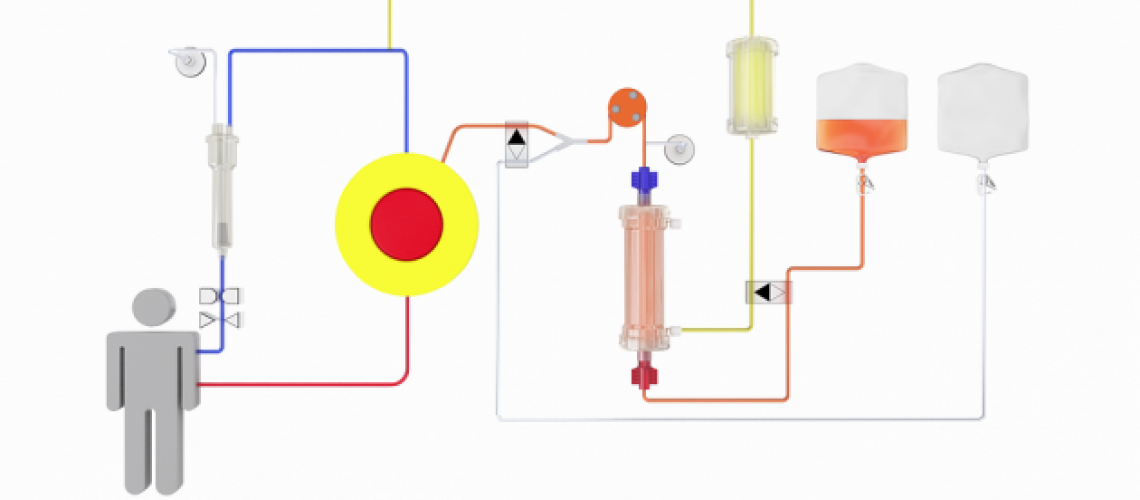
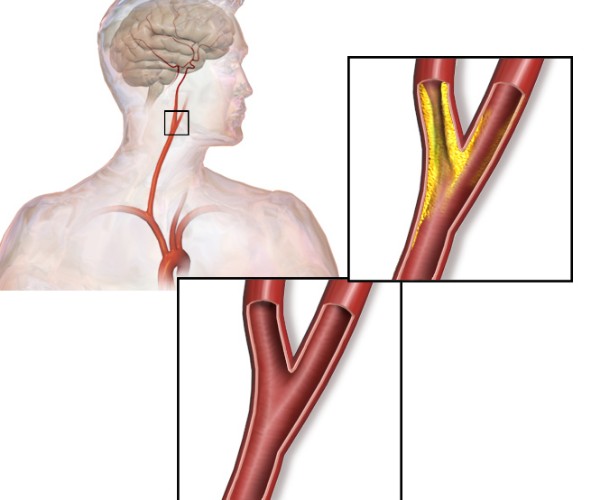
This is a system in which blood is brought from the patient, by arterial cannulation, into an extracorporeal circuit. The blood, before returning to the body via the venous route, is cleansed of toxins. Nonionic resins and activated charcoal in granular form are used to perform hemoperfusion .
Just as with hemodialysis, hemoperfusion does not can speak of a universal answer to all problems facing the clinician toxicology. It should be limited only in certain cases:
- The adsorbent has an affinity for the toxin
- The amount of circulating toxin must be a good portion of that contained in the body
- There is a correlation between the concentration plasma toxin and the intensity of poisoning.
Hemoperfusion is contraindicated when:
- The toxin has a large volume of distribution
- The natural metabolic inactivation of the toxin is able to proceed faster than the time it takes for staff to health care to proceed with hemoperfusion
- The toxic mechanism is precise and quick.
Hemoperfusion is, therefore, indicated, when:
- No other methods of treatment
- The toxin that threatens the patient has a small volume of distribution in the body
- The substance has been analytically identified in the blood.
Techniques
Performing a hemoperfusion requires the cooperation of experienced people, as it requires the same degree of experience that is needed for hemodialysis. Facilities must be available to measure drug concentration in the palsma so that electrolyte balance, heparin levels, and other hematologic parameters can be repeatedly checked.
A fall in leukocyte and blood platelet values is possible. Random bleeding can be worrisome and even disastrous, so even minor surgeries should be performed with caution.
Source: Roy Goulding’s Vademecum of Poisoning Therapy.