Antibiotic resistance, that is, the growing ability of pathogenic bacteria to survive in the presence of the drugs that are supposed to kill them, is one of the greatest challenges facing medicine today and on whose victory the chances of survival of humankind in the coming decades depend.
For those born in the era of antibiotics, it is difficult to realize this emergency, but to find oneself out of the blue without medication that can fight infectious diseases as severe as tuberculosis, pneumonia or bacterial gastroenteritis means being exposed to a very high risk of epidemics capable of claiming millions of lives and extremely difficult to contain.
In an effort to limit the spread of bacterial resistance, for more than two decades, the World Health Organization and other health institutions internationally recommend using antibiotics cautiously, sparingly, and properly: that is, only when essential, at the dosages and for the time period prescribed by the doctor, and never on a do-it-yourself basis.
However,antibiotic resistance can also be promoted in non-health care settings. The best known of these is animal farms, where antibiotics are often used to protect livestock from infection. New evidence now indicates that the hygiene of closed environments such as homes and offices can also facilitate the selection of “super-bacteria.”
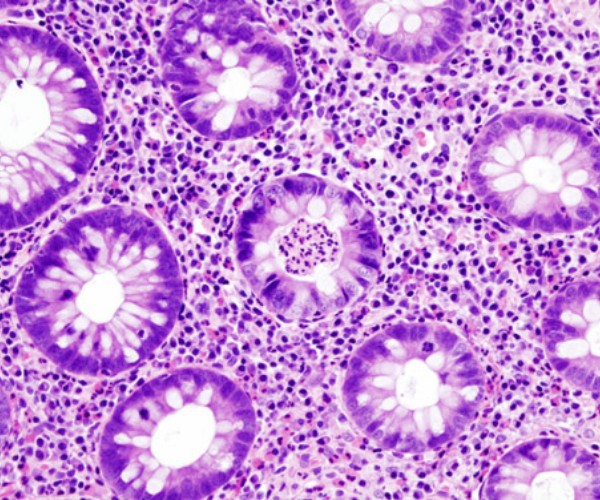
Specifically, research recently published in the scientific journal Nature Communications reports that in the enclosed rooms of buildings of any type, the biodiversity of bacteria is less than that typical of the outdoor environment (urban or natural), and that the strains less sensitive to commonly used antibiotics are more likely to be represented.
According to the researchers, this finding may be a consequence not only of the type of occupancy and human activities carried out in the buildings and the more or less pronounced isolation from the outside environment, but also of the products and methods used to clean the surfaces. In particular, it is hypothesized that theuse of broad-spectrumantibacterial detergents may play an unfavorable role, rewarding the “stronger” bacteria that would be able to multiply prevalently.
Given that domestic cleanliness, the premises and buildings frequented by many people is indispensable to prevent diseases and hygiene problems of various kinds, to avoid promoting bacterial resistance in enclosed environments, researchers suggest alternating the cleaning substances used (so that bacteria cannot habituate) and reserving overtly antibacterial products for circumscribed places deserving of increased disinfection (bathrooms, kitchen countertop, garbage compartment, etc.).
Other useful measures include using steam to sanitize surfaces that can tolerate high temperatures, putting plants in rooms (avoiding those most at risk of allergies), and increasing indoor-outdoor exchanges (for example, opening windows often).
Source
Mahnert A et al. Man-made microbial resistances in built environments.
Nature Communications 2019;10:968. doi:10.1038/s41467-019-08864-0 (https://www.nature.com/articles/s41467-019-08864-0)