The term acne comes from the Greek word acmé or acné, meaning foam or summit. It is one of the most common skin diseases in the juvenile population; in fact, it is present in about 95%. The frequency is much higher certainly among adolescents, but acne can persist or appear in adulthood as well.
Types of acne
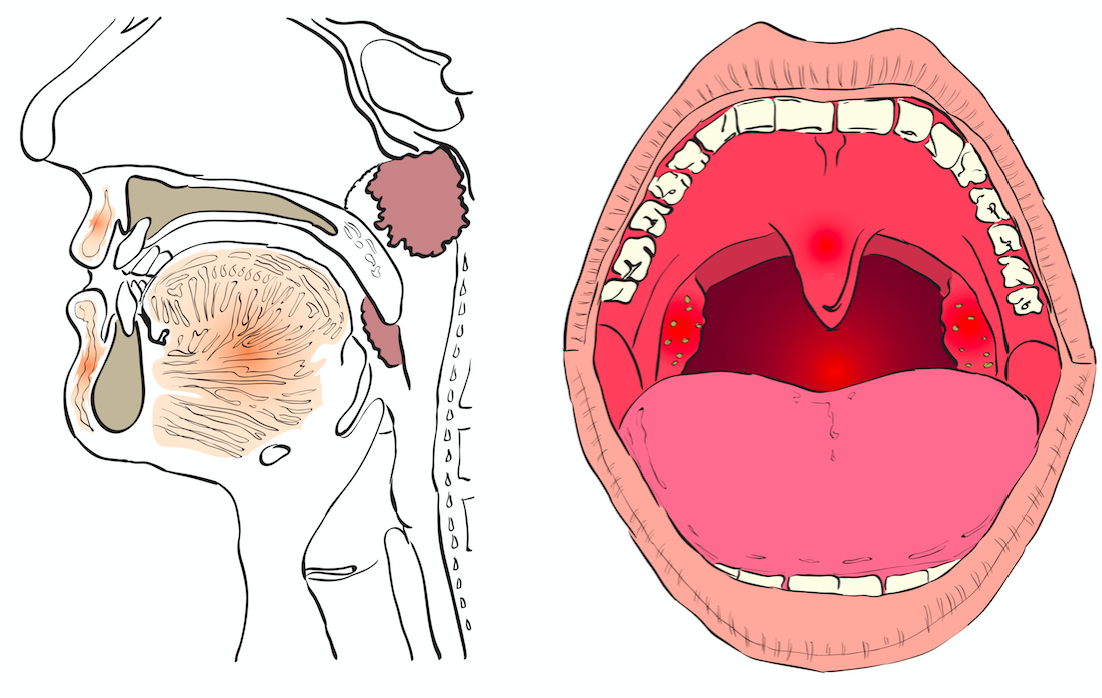
It typically makes its onset on the face, back, chest, and shoulders and affects both sexes in almost similar percentages. It typically manifests as closed and open comedones, so-called blackheads, papules, or whiteheads, pustules, better known as pimples, nodules i.e., furuncles, cysts, and unfortunately can also result in scarring in some cases. There are many causes of acne: increased activity of sebaceous glands, thickening of the wall of follicular ostium, bacterial colonization, in pjoint by Propionibacterium Acnes, and inflammation. In addition, various factors contribute to its occurrence such as family predisposition, stress, and smoking.
Especially in adolescence, it is important to be able to frame the degree of acne early, that is, whether it is mild, moderate, or severe, or, depending on the type of lesion, it can be classified into comedonic, papulo-pustular, nodular, and, in severe cases, conglobate. This avoids the development of scarring. In fact, this condition is often underestimated, which can therefore lead to psychological distress on the part of young patients and delay the benefits of treatment. It is known from studies conducted on patients’ quality of life that the acne-prone adolescent often suffers from low self-esteem, embarrassment, shyness, and in extreme cases even depression, emotional turmoil, shame about one’s appearance, resulting in difficulty relating to the opposite sex and a decline in school performance.
Therapies
Regarding treatment, the European Guidelines, published in 2012 recommend which drugs, topical and systemic, to use according to the degree of acne. Topical retinoids, derived from vitamin A, are the first choice in comedonic acne. An important role is also played by benzoylperoxide a keratolytic agent with antibacterial action but not inducing antibiotic resistance, which is recommended in acne vulgaris and comedo- or papulo-pustular-predominant forms.
The use of topical antibiotics is useful in inflammatory forms, but is limited by resistance, which unfortunately is increasing in Europe. therefore, as far as acne is concerned, their local use in combination with other topical drugs is advisable, avoiding the concomitant administration of oral antibiotics and limiting the use of the latter to periods not exceeding three months, discontinuing them if there is no improvement. Remembering to fixed combinations of topical preparations offers the possibility of acting more specifically on the mechanisms that cause acne, also increasing adherence to therapy, making the application of only one product sufficient.