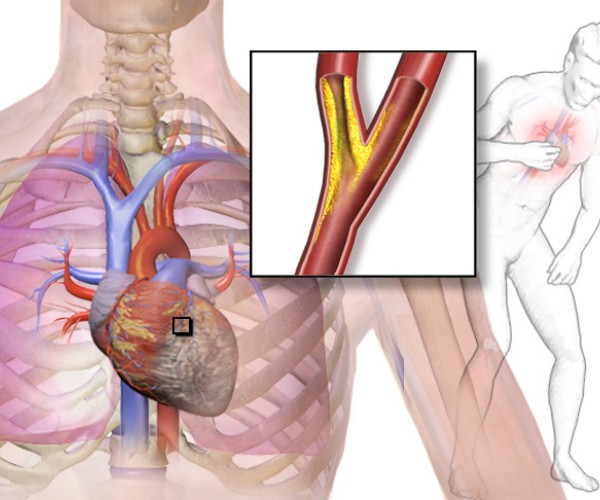
Congenital long QT syndrome is a cardiac condition present from birth that essentially consists of a “repolarization defect,” that is, an electrophysiological alteration that results in a lengthening of the time required for the cells of the heart to “recharge” after contraction of the ventricles. The name of the disease comes from the fact that this increased repolarization time can be seen on the electrocardiogram (ECG) tracing as the elongation of a particular segment called precisely “QT.”
By itself, long QT syndrome gives no symptoms and for this reason is poorly diagnosed, except during electrocardiograms required for other reasons, such as preoperative examinations, pre-sports check-ups, apparently unmotivated fainting spells, or other cardiological disorders. Unfortunately, when it occurs it does so in a striking manner, with ventricular fibrillation, cardiac arrest, and sudden death. Triggering these effects can be a very intense physical exertion or emotion or a fright or sudden awakening in the middle of the night. But sometimes fatal arrhythmia can also occur during sleep.
To date, there is no real cure for long QT syndrome, but there are some steps that can help reduce the risk. Among these, a very important one concerns medications that may need to be taken throughout life for a wide variety of reasons: from antibiotics to analgesics, from antacids to antidepressants. Many commonly used drugs, in fact, tend to have a “pro-arrhythmic” action, that is, to promote transient alterations in heart rhythm. In people without long QT syndrome, this generally does not create particular problems (except perhaps some palpitation during therapy). In contrast, if a person with long QT syndrome is taking a pro-arrhythmic drug, the risk of ventricular fibrillation and sudden death are significantly increased.
For this reason, the European Society of Cardiology (ESC) guidelines dedicated to this condition have long and strongly recommended that drugs known to be pro-arrhythmic should not be prescribed to sufferers, opting, where possible, for alternative therapeutic solutions without cardiac effects. In clinical practice, however, these recommendations seem to be largely disregarded. In particular, a recent Danish study indicates that 60% of people with congenital long QT syndrome are prescribed pro-arrhythmic drugs in the years after diagnosis, even for prolonged periods.
The most prescribed “arrhythmia risk” drugs were found to be some antibiotics (such as azithromycin, clarithromycin and erythromycin; 34.1 percent), antacid proton pump inhibitors (esomeprazole, lanzoprazole, omeprazole, pantoprazole; 15.0 percent), antidepressants (citalopram, escitalopram, sertraline; 12.0 percent) and antifungals (fluconazole; 10.2 percent). Those considered in the study were less likely to be prescribed pro-arrhythmic drugs in the year following the diagnosis of congenital long QT syndrome than in the previous year, but not by much (28.4 percent vs. 23.2 percent), while in more than one-third of the cases (33.5 percent) the at-risk drug therapy was still ongoing after five years. The likelihood of prescribing risky drugs increased slightly with age and multiplied by more than 2.5 times when the same drug had been taken by the patient before (probably, on the basis of erroneous reassurance with respect to possible cardiac side effects).
Although the study did not show a correlation between pro-arrhythmic drug use and increased mortality from ventricular arrhythmia or all causes, the authors and ESC experts urge greater caution on the part of physicians when prescribing potentially high-risk drug therapies in those with congenital long QT syndrome. On the other hand, even patients with a known diagnosis should remember to always inform any specialist physicians they spontaneously visit for consultations in various clinical settings of the cardiac issue they are suffering from, to enable them to identify optimal and safe treatment strategies.
In addition, those suffering from congenital long QT syndrome should always seek advice from their physician and/or pharmacist even when it comes to choosing commonly used over-the-counter drugs that are generally considered safe and manageable: although they indeed are for most people, some of them may be contraindicated in those who are genetically predisposed to cardiac arrhythmias (this is the case, for example, with some antihistamines).
Source:
Weeke PE et al. Long-termproarrhythmic pharmacotherapy among patients with congenital longQT syndrome and risk of arrhythmia and mortality. European Heart Journal 2019;40, 3110-3117. doi:10.1093/eurheartj/ehz228(academic.oup.com/eurheartj/article/40/37/3110/5488147)