HOW TO RECOGNIZE IT
Regurgitation is the involuntary rising of gastric contents into pharynx, inside or outside the mouth, usually effortless and nonprojective. One aspect to be differentiated immediately from regurgitation is gastroesophageal reflux (GER), which is also physiologically frequent and often associated with oral regurgitation. Regurgitation is as common as ever: it is estimated to affect more than 50% of infantsaged 3 to 4 months with daily frequency, and at least four episodes occur daily in 20% of cases.
Unlike gastroesophageal reflux disease, regurgitation does not lead to complications, but it evokes considerable anxiety in parents and is responsible for many pediatric visits: about one in five parents, in fact, seek help with frequent regurgitation. For this reason, despite a favorable prognosis, it is not at all uncommon for infants with regurgitation to undergo major interventions, such as dietary modifications (changing the type of formulated milk) and even pharmacological treatments of questionable benefit. A further concept to be clarified is rumination, defined as voluntary, habitual and effortless regurgitation of recently ingested food.
Uncomplicated regurgitation in an otherwise healthy infant is considered a developmental stage and not a disease. In fact, more than half of healthy infants have daily episodes of regurgitation, and only a small percentage are still present at 10-12 months of age.
ASPECTS TO BE EVALUATED AND REPORTED
- Daily number of episodes;
- distance from feeding;
- Character of the material emitted (is it acidic or not?);
- Infant growth;
- Any “reactions” of the infant after the episode (e.g., crying, change of position).
Suspicious elements are:
- regurgitation becomes persistently jet-like (vomiting);
- Vomiting is bilious (green or yellow-green) or with blood;
- New signs/symptoms such as agitation or major irritability, feeding difficulties or stunting appear;
- regurgitations persist beyond one year of age.
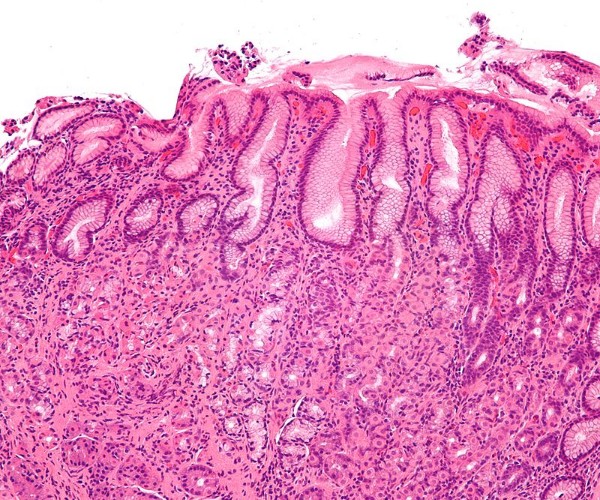
CAUSES AND MECHANISMS
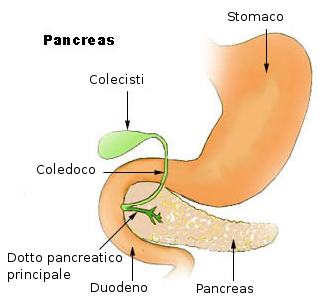
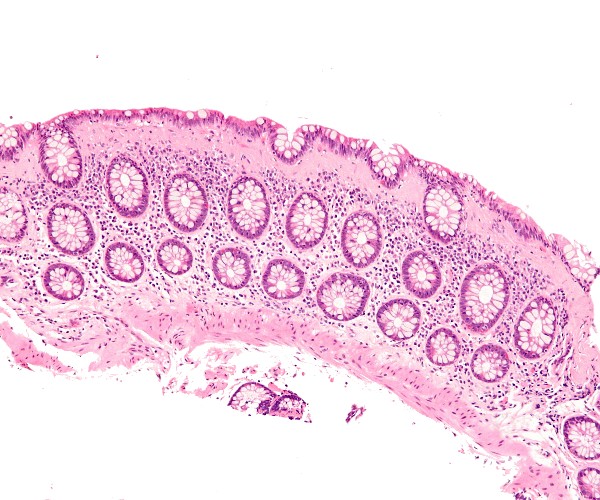
Regurgitation can be promoted by several predisposing factors (predominantly supine position of the infant, reduced tone of the cardia, the valve interposed between the esophagus and stomach), but it has no pathological significance. Indeed, in cases of very voracious infants, it is even considered a protective system against ingesting an excessive volume of milk. Regurgitation and reflux should also be differentiated from vomiting, understood as a coordinated autonomic and voluntary motor response with forced expulsion of gastric contents from the mouth, and gastroesophageal reflux disease, which is the pathological expression of reflux with manifestation of symptoms or complications.
CARE AND PREVENTION
Excessive regurgitation, usually characterized by more than four episodes per day, is often a cause of concern for parents but should not be confused with gastroesophageal reflux disease, as it is neither a sensitive nor a specific symptom, but most often physiological and spontaneously resolving in the first year of life. However, it is worth mentioning that sometimes frequent regurgitation may be an expression of other conditions that need to be properly ruled out, such as food allergy, infection, respiratory or neurological diseases. Regurgitation physiologically reduces with time (it resolves in 90% of infants before 1 year of age) and usually does not need further investigation or treatment. In some cases, the pediatrician may suggest the use of an “AR” (anti regurgitation) milk, a formula appropriately thickened to precisely counteract regurgitation after feeding.