We live in a society that is now considered by many to be “postmodern” and in which an exclusively technical approach to medical care is no longer considered sufficient. Twenty-first-century patients seek a different approach to their health problems than in the past, and in particular demand a deeper dialogue with their physicians (Shapiro, 2011; Greaves, 2004).
Medicine can no longer be limited to collecting a medical history (anamnesis), performing an objective examination, and implementing a diagnostic procedure with a final discussion of therapeutic intervention strategies (Johna et Dehal, 2013). Medicine especially needs physicians capable of establishing narrative connections and more intense contact with the person asking for help (Charon , 2001). Narrative medicine aims to deal with patients comprehensively and to recognize and interpret their stories of illness by integrating education, medicine and the humanities (Frank A, 1995). The goal is to strengthen the doctor-patient relationship by providing more humane and ethical care.
The narrative
With narrative medicine, we seek to understand the patient-physician relationship through the collection and analysis of narratives, told from the perspectives of the different stakeholders, patient, civil society, health care facilities, physicians and family members (Charon, 2012). This practice uses methods aimed at obtaining information about how a person experiences his or her illness, in an effort to consider the many facets of the care journey: narratives allow health professionals to gather information about the patient’s perceived needs on how to cope with problems related to his or her health.
Empathy
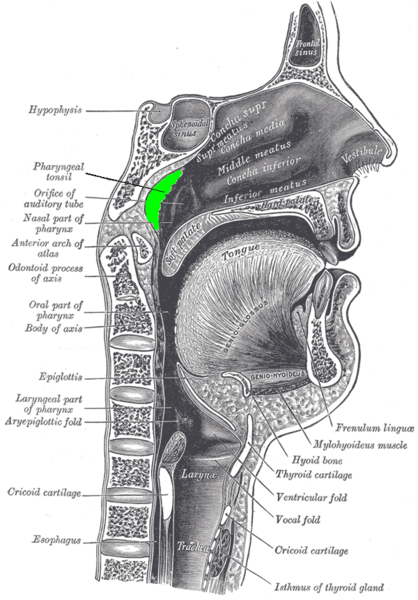
Although objectivity and medical care always retain their importance, a good deal of empathy is asked of the physician that will be rewarded by greater patient satisfaction and better clinical outcomes. What is empathy? It has been defined as a psychological process that enables an individual to have feelings that are more congruent with others as well as himself: it is basically the ability to understand and share others’ feelings. Empathy can be distinguished into cognitive, which is the ability to understand how another person feels, and affective, which is experiencing the same emotions that the other person feels (Hoffman, 2000; McDonald et al. 2015).
The negative aspects of the traditional approach
At present, the doctor-patient relationship is overwhelmingly based on scientific aspects, a position corroborated by the biomedical innovations that have occurred over time, from antibiotics to organ transplants, and which have made it possible to solve many health problems. Medical examinations tend to be always and only “scientific”: diagnosis is based on objective parameters, treatment centered on clinical protocols closely related to scientific research, and consequently the patient’s “well-being” will be linked only to the achievement of certain standard goals.
All this fails to consider that medical practice is above all a human endeavor and that each patient is his or her own case. The patient’s history, the so-called anamnesis, is reduced to repetitive, routine sentences, whereas the human case should be the focus of clinical practice. (Montgomery, 2006). Narrative medicine makes it possible to view individual subjects as persons rather than clinical cases, to understand the world in which they live, and to tailor drug treatment to their needs. Both the patient and all caregivers, including caregivers, will be taken into account.
The goal: to improve patient care by enhancing both medical science and human aspects. Only in this way can the person be assisted as a whole and in a more meaningful way (Franke RJ, 2016). Narrative medicine fosters empathy and trust between patients and patients and between patients and physicians by improving communication with effect a therapeutic on patients. It is used in individuals with cancer, AIDS, stroke, and generally chronic diseases, but also in seemingly more mundane conditions, such as chronic spontaneous urticaria (Cappuccio et al, 2017). Another area of application is palliative care, treatment given to people at the end of their lives.