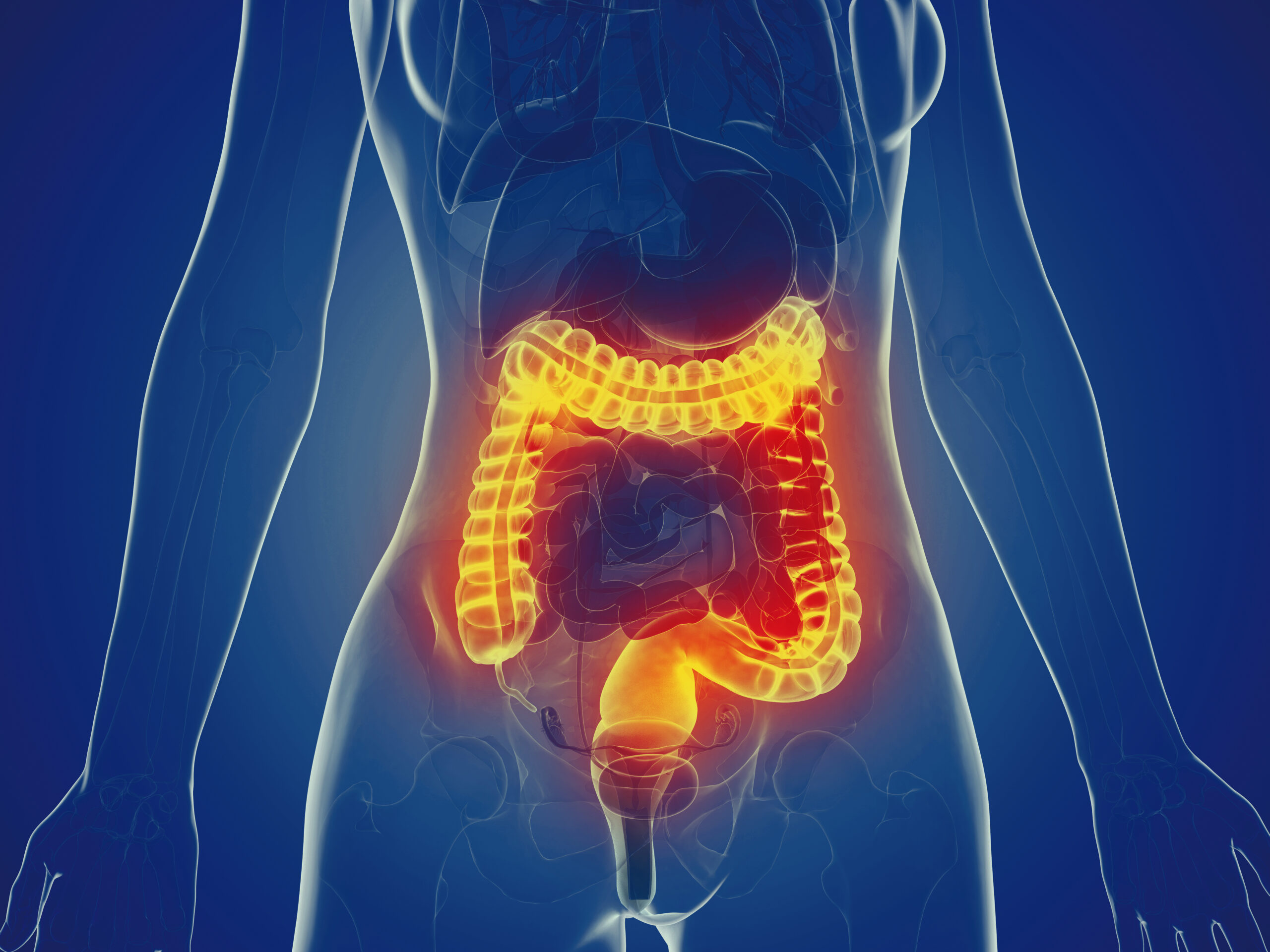
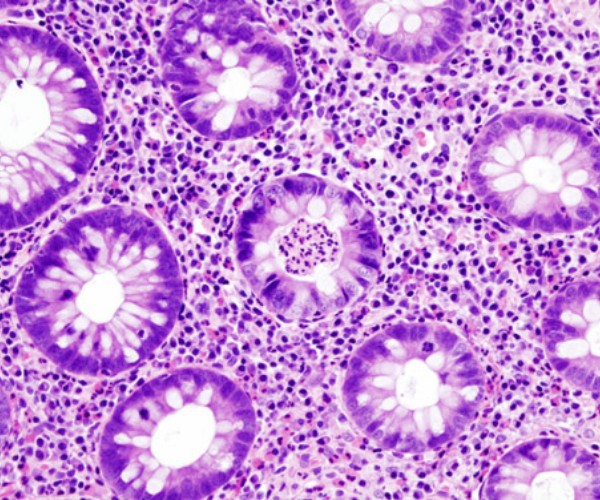
Medicine, accustomed as it is to conventions and classifications, distinguishes diseases into organic and functional. The former are those associated with actual damage: this is the case, for example, with gastroenteritis caused by infection by a bacterium or virus, which settles in the intestines giving rise to diarrhea. Functional diseases, on the other hand, despite the occurrence of sometimes even intense symptoms, are characterized by the absence of injuries documentable: diarrhea, to refer to the situation just hypothesized (but an entirely similar consideration applies to the diametrically opposite condition, constipation), is triggered or maintained by factors that are not clearly identifiable or quantifiable, such as a particular emotional state.
Gastrointestinal functional disorders
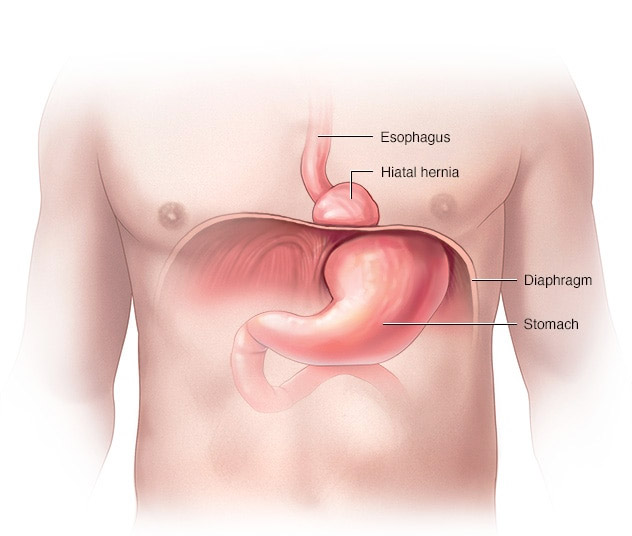
What then are functional gastrointestinal disorders? They can be defined as a set of recurrent or chronic, age-varying symptoms that are independent of an underlying disease. In the first 2 years of life they may be physiological, that is, an expression of normal development, such as infant regurgitation, or, later, they may result from abnormal behavioral responses to internal or external stimuli, such as functional constipation caused by painful defecation.
Thus, at the basis of functional gastrointestinal disorders we find physiological, psychological and sociocultural factors capable of amplifying the perception of symptoms, which are experienced as severe, disabling and burdened with major repercussions on daily activities. Examples of functional disorders, in addition to those mentioned above, include colic, cyclic vomiting syndrome, and dyschezia (pain at the time of stool emission) in early childhood, abdominal migraine, functional dyspepsia, and irritable bowel syndrome in preschool, school, and adolescent ages.
Diagnosis and treatment
Two other elements need to be highlighted: first, there are no diagnostic indicators. In other words, there are no laboratory tests or benchmarks to be able to make the diagnosis, which is therefore based on as objective a set of symptoms as possible. Secondly, the care cannot be limited to medication but requires an approach that takes into account genetic and environmental factors (family influences, emotionally important events, infections, and so on), which may influence the child’s psychosocial development and cause him or her to be more susceptible to stress or bowel dysfunction (altered motility, altered immune system or visceral hypersensitivity). If, for example, a child suffers from functional diarrhea, treatment will have to contemplate the use not so much of medication but of dietary and especially behavioral measures, both for the child and his or her family members.
In the current view, in short, every intestinal disorder deserves to be transcoded not under the trivial label of a pretext contrived by the child to avoid a challenging test, but in the logic of a more complex effect resulting from the interaction between the organic sphere and the environment.