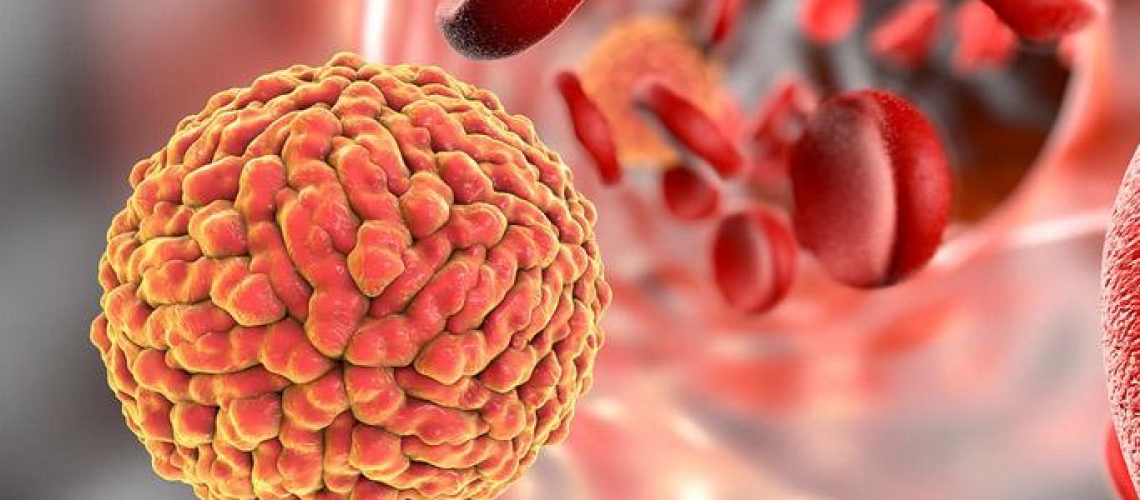
Two years ago, the Zika epidemic had terrified pregnant women residing in regions endemic to the virus, such as Brazil and even parts of the United States. Their fear was justified by the link between Zika virus infection during pregnancy and the risk of some serious birth defects in the unborn child, particularly the condition known as microcephaly, in which there is incomplete skull development, mostly accompanied by mental failure.
The absence of early prenatal diagnosis or treatment has led to enormous concerns and numerous pregnancy terminations. Fetal MRI captures high-resolution snapshots of the fetus, but this imaging technique can be used only in the second or third trimester, when terminating a pregnancy is more complex.
At University of Southern California, a team of researchers is studying the mechanisms behind the devastating consequences of Zika with the goal of developing new prenatal diagnostic tests that can determine whether babies will be born healthy and now, as can be read in their study published in JCI INsight, have taken a significant step forward.
“Our results,” the authors write in The Conversation. – revealed an elevated production of 16 specific protein biomarkers found in the blood of pregnant women who gave birth to children with developmental delays and ocular abnormalities. These biomarkers are potentially useful for predicting Zika pregnancy outcomes simply by using blood samples from the mother-to-be at any stage of pregnancy.”
The number of Zika cases has decreased dramatically following the decline of major outbreaks in 2016, yet many children are still suffering from the terrible consequences of prenatal infection. And the risk of new outbreaks is by no means averted, as the Zika virus has not been eradicated and Aedes mosquitoes-which are its transmission vector-are still widely spread.
Source: Foo SS et al. Biomarkers and immunoprofiles associated with fetal abnormalities of ZIKV-positive pregnancies. JCI Insight. 2018 Nov 2;3(21).