Insomnia, hypertension and diabetes: watch out for those three!
Recent studies have shown that there is a close correlation between sleep disorders and diseases of the cardio-metabolic system, such as hypertension and diabetes. According to the numbers, 4 out of 5 diabetic patients And 2 out of 5 hypertensive patients frequently present with symptoms of insomnia. The question from those who have this disorder is as follows: I can’t sleep.
This confirms the theory that alterations in the internal biological clock can adversely affect some of our body’s basic physiological functions, affecting not only performance and mood, but also hormone levels, body temperature, blood pressure and energy metabolism.
According to research, insomniac individuals have a 300-500% higher risk of high blood pressure than non-insomniac individuals, regardless of age, body mass index, diabetes, alcohol consumption and smoking. Probable cause of the link between sleep disorders, hypertension, and diabetes could be a low melatonin level, a natural hormone produced in the pineal gland that regulates circadian rhythms and the proper functioning of our internal biological clock over the 24 hours. In addition to acting on the sleep-wake rhythm, in fact, melatonin has a direct action in regulating energy and glucose metabolism. Moreover, by acting on circadian rhythms and consequently on blood pressure, it can also affect the cardiovascular system.

Intervening on sleep disorders can be instrumental in improving one’s overall health. And it is in this context that, thanks to the contribution of Fidia Pharmaceuticals, continues the Sleep & Health Project, in its second edition, whose goal, under the auspices of the World Sleep Society and with the support of Italian associations and scientific societies, is a Early identification of patients with insomnia or other sleep disorders, in order to set them on a suitable course of treatment.
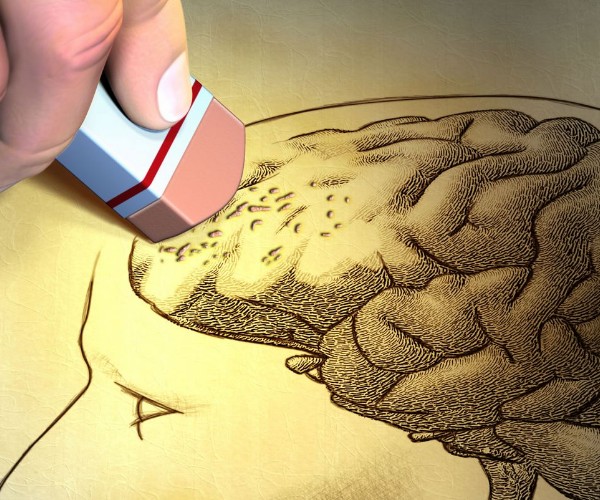
The first step in treating insomnia is definitely behavioral and aims to correct habits, expectations, and conduct that may trigger or maintain the disorder. As for drugs, the following are frequently used sedative-hypnotics with a short half-life and 2 mg of melatonin extended-release. It is preferable to use sedative-hypnotics for short periods, no more than four weeks, because they tend to lose their effectiveness if taken systematically every night for a long time; in addition, chronic intake can have negative effects on sleep structure itself as well as on daytime vigilance levels and some cognitive functions such as memory and attention.
In contrast, the administration of extended-release melatonin 2mg is especially recommended for insomniacs over the age of 55. The treatment is non addictive and is approved for 13 weeks’ continuous administration, even with other therapies for the treatment of hypertension and diabetes.