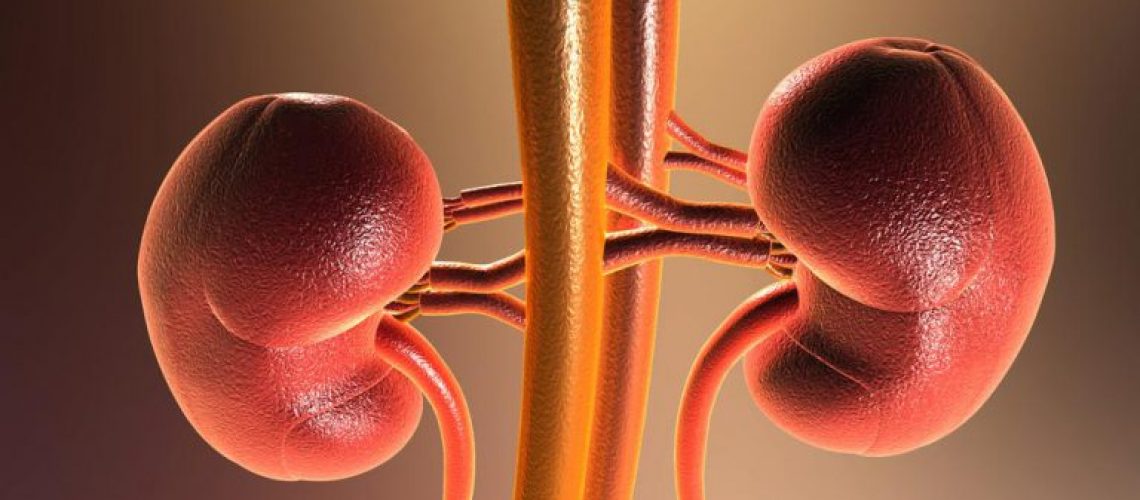
Chronic kidney disease is often clinically silent, and conventional clinical data alone do not allow differentiation of disease subtypes, but the results of a recent study supports the use of genetic analysis to improve its diagnosis and treatment.
In clinical practice, diagnosis and monitoring of chronic kidney disease are based on clinical parameters and only rarely involve renal biopsy. However, in many cases the disease occurs in a “silent” form and is difficult to discriminate using clinical data alone.
Thus, in many individuals, the precise cause of progressive damage to the kidneys remains unknown and the diagnosis is made late, reducing the opportunity for early therapeutic intervention; moreover, few of the current treatment approaches are individualized, but according to the study published in the New England Journal of Medicine, genetic testing could help overcome these critical issues.
The authors performed exome sequencing (the set of all portions of the genome that “code” for proteins) of 3,315 patients with chronic kidney disease due to different causes and reported a 9.3 percent rate of diagnostic genetic variants, comprising 66 monogenic sites already known to be associated with kidney disorders.
“This study,” reads an editorial in Nature Reviews Nephrology. highlights the potential of genetic testing for adults with chronic kidney disease and end-stage renal disease (Esrd). Discovering the underlying genetics of different forms of kidney disease will serve to improve diagnostic accuracy and develop new approaches according to “precision medicine.” Obtaining a genetic diagnosis for a patient with chronic kidney disease could improve clinical management, including choice of therapy, and enable targeted disease surveillance. Deepening the genetic basis could also reveal new biological mechanisms associated with the disease and lead to defining new therapeutic targets that could benefit a large number of patients.”
Groopman, EE et al. Diagnostic utility of exome sequencing for kidney disease. N Engl J Med. 2019 Jan 10;380(2):142-151.