Theoutbreak from Covid 19, first developed from localized outbreaks, then spread across nations and continents, transforming into a pandemic, starting in late 2019, and then “escalating” from early 2020.
All countries and nations are waiting for a cure, a remedy, a shield that can halt the advance of this virus that is undermining not only the physical health of populations, but also their mental health, and bringing with it devastating consequences for people’s work, economy, and social and family life.
The common sentiment today is one of waiting for a vaccine, to prevent coronavirus disease (COVID-19) and also to end the pandemic.
In recent days, news reports from all countries have announced the imminence of a new vaccine produced in the U.S. that would have a 90 percent efficacy level, but there is also talk of several other vaccines, including one produced in the UK by an Anglo-Italian collaboration, and some others based on different technologies.
There are so many questions about which one will be the most effective, which one will be the least risky, or the one that can provide long immunization, or even which among these vaccines will be best storable and transportable to provide to all populations.
It will be necessary to wait a few more weeks for more clarity and for the many questions to be answered.
Research on an effective vaccine against Covid 19 has been ongoing for months by scholars, laboratory researchers, university institutes, pharmaceutical companies, and by the Health Authorities of many countries.
An effective COVID-19 vaccine will need to provide people with long-term protection from infection. Protecting the elderly.
But how many types of vaccine is research trying to study, and which among them might be the most effective against Covid 19?
- There are live vaccines ( such as measles vaccines ) that require extensive studies to be certain of safety for human use, since the live germ contained nonetheless produces an infection.
- Then there are inactivated vaccines, which contain a killed germ that is only capable of generating an immune reaction. For all vaccines, the lead times are considerably long, as they take place over several stages, starting with animal testing and ending with controlled administration to humans.
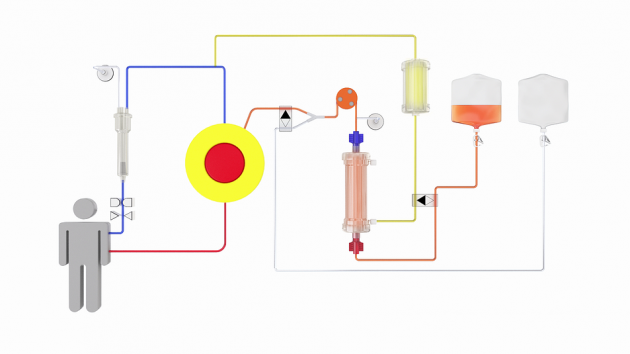
Theurgent need to develop an effective vaccine to ensure immunity against COVID-19 infections has prompted some research centers to use a different technology for vaccine research and production: messengerRNA(mRNA) technology, realizing a different pathway in vaccine creation.
But how does this technology work?
RNA ribonucleic acid, as well as DNA is a nucleic acid actively present in various biological coding and is a key player in protein synthesis.
ThemRNA (or also messenger RNA) transmits on behalf of DNA genetic data and information for protein construction.
Some explanatory premises need to be made:
- Coronaviruses are a type of virus mainly responsible for colds, also for the acute respiratory syndrome, Sars, and the respiratory crisis known as “eastern,” Mers.
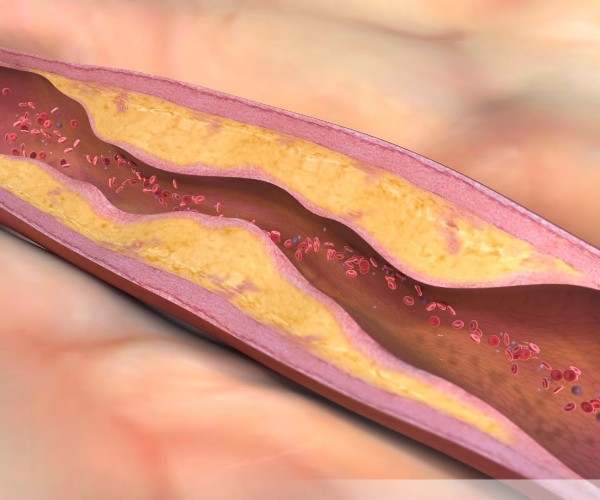
- This virus has its own spiky, spear-like structure called the S protein, so the many spikes give the virus the appearance of a crown, hence the name. The S protein is like a system by which the virus latches onto human cells to reproduce.
- The goal of the vaccine is to deprive the virus of the protein, called the Spike protein to prevent it from attacking the cell and reproducing.
- The studies, which are still ongoing, aim to assess the vaccine’s safety, level of adverse reactions and level of immune response.
- A vaccine based on such sophisticated technology, if tested and approved for safety in humans and efficacy against Covid 19, would represent the opening of a new scientific avenue against this epidemic and the dispatch of brand new vaccine technology procedures, hitherto unknown.