In a recent article (Liang H, Acharya G. Novel corona virus disease (COVID-19) in pregnancy: What clinical recommendations to follow? AOGS 2020; doi.org/10.1111/aogs.13836) discussed clinical recommendations in pregnancy during this time of the Corona-virus pandemic.
However, it is important to highlight how these recommendations refer to guidelines that evolve as more and more data become available and new experiences are gathered. The same Interim Guidance on the Management of COVID – 19 issued by the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) includes recommendations for pregnant women based mainly on the experience of previous outbreaks.
A multidisciplinary approach would be needed for the management of these patients, enabling communication and sharing of expertise and responsibilities.
The important starting premise is that because pregnancy is a state of partial immune suppression, pregnant women may be more vulnerable to viral infections. It would therefore be desirable and advisable for them to adhere to appropriate social distancing as well as personal and social hygiene rules. Should you experience symptoms such as fever, sore throat, cough, fatigue, myalgia, shortness of breath you should promptly consult your doctor. If any woman has had contact with infected people or has traveled to an area with a high incidence of infection, she should be placed under observation and in isolation. Attention should always be paid, however, to mood and have the opportunity to offer professional psychological support if necessary, since anxiety and depression can develop during pregnancy.
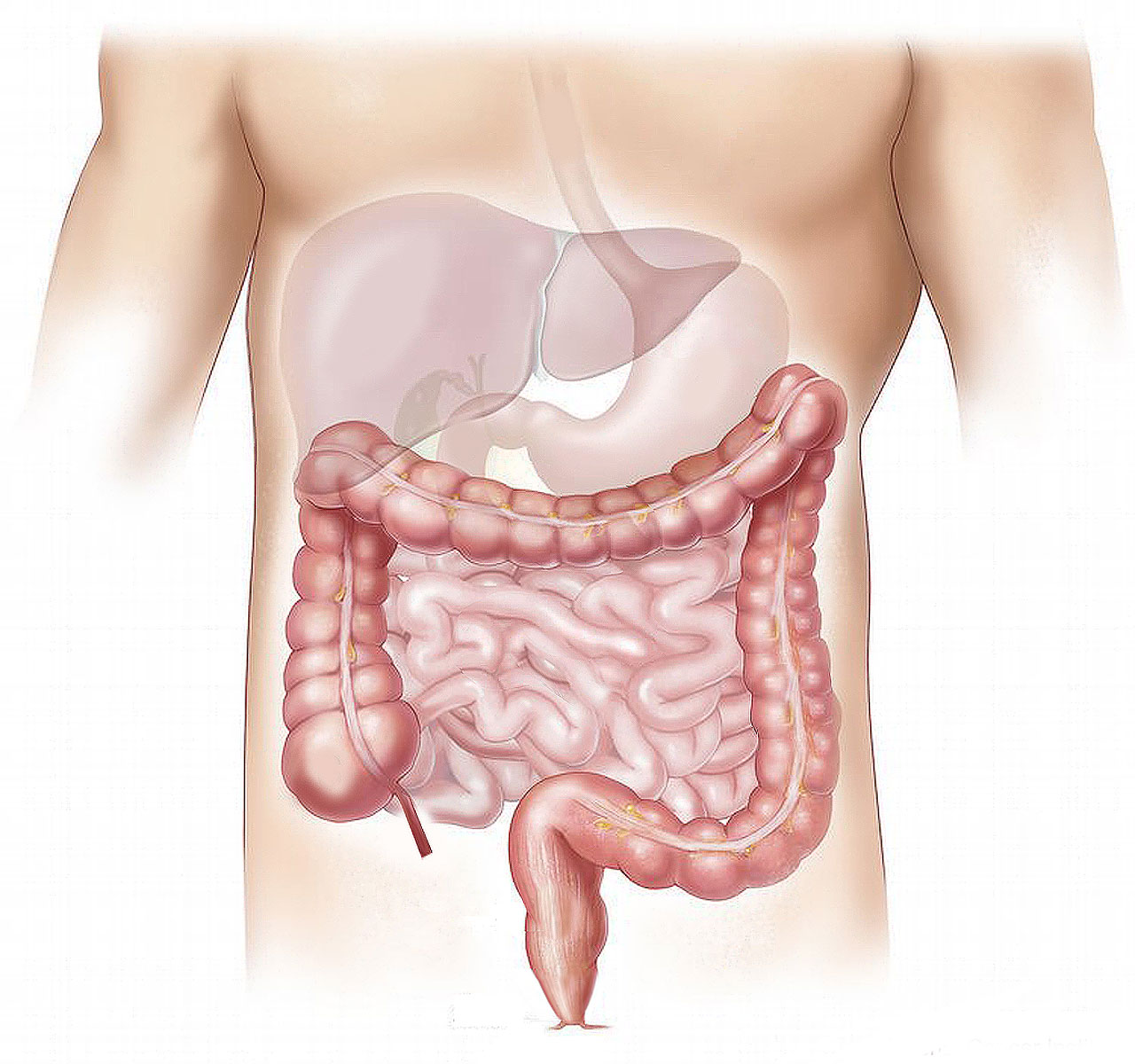
In suspected cases, tests (with samples obtained from saliva, upper respiratory tract, lower respiratory tract, urine and feces) should be repeated to confirm the diagnosis. In addition, a noncontrast computed tomographic (CT) scan of the chest is the most useful investigation both to confirm or rule out viral pneumonia and because fetal radiation exposure is very low.
People diagnosed with infection should be admitted to an isolation ward, where adequate rest, hydration, nutritional support, water and electrolyte balance, and constant monitoring of vital signs and oxygen saturation can be ensured.
Pregnant patients can be given antiviral treatment; antibiotics are to be given only in the presence of a secondary bacterial infection. In contrast, the use of corticosteroids is not recommended.
Regarding the course of pregnancy, there is not enough information when the infection occurs in the first or second trimester. Instead, it would appear that if the infection occurs in the third trimester, there may be risk of premature rupture of membranes, preterm delivery, tachycardia, and fetal distress.
Regular monitoring of maternal vital signs, ultrasound examination and heart rate monitoring is necessary to assess fetal well-being. Based on obstetric history, gestational age, and fetal condition, a decision may be made to continue the pregnancy to term under close supervision. Conversely, in the face of severe infection, existing comorbidities such as preeclampsia, diabetes, heart disease, etc., it may be necessary to “tailor” the timing of delivery. If continuation of the pregnancy may pose a risk to the survival of the mother or the safety of the fetus, it is appropriate to proceed with delivery, even if prematurely. In particularly critical cases, to save the woman’s life, a decision may be made to terminate the pregnancy after, of course, careful discussion with the patient, family members, and the ethics committee.
As there is no evidence related to transplacental and vertical transmission ( Amniotic fluid, cord blood and neonatal throat swab in babies born to positive mothers are negative) there is no contraindication in stable patients to vaginal delivery. If a cesarean section is to be used, attention should be paid to the choice of anesthesia.
While, as mentioned above, transplacental transmission is unlikely, infection can occur with close contact between the infected mother and the infant. In these cases, therefore, it is first recommended that the umbilical cord be cut quickly and that the child be placed in isolation for at least two weeks and monitored for signs of infection.
Breastfeeding is discouraged, precisely to avoid direct contact, while breast milk draught is recommended, since breast milk samples tested negative for SARS-COV-2.