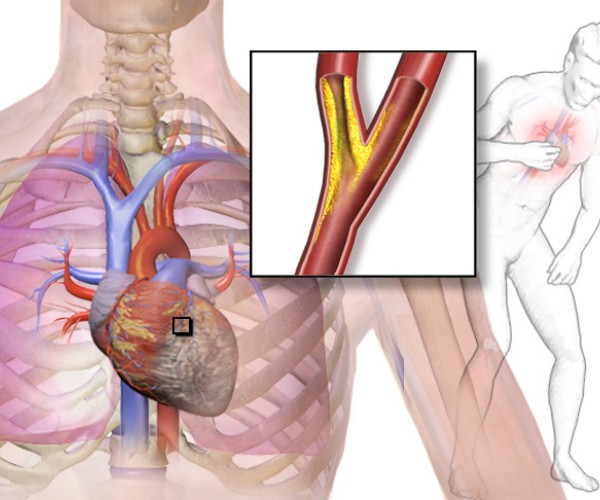
A coronary stent is a medical “device,” that is, an instrument used in Coronary Angioplasty to clear the way for possible blockages in the coronary arteries by following invasive techniques having the goal of restoring regular blood circulation within the heart by ensuring its proper function.
Causes
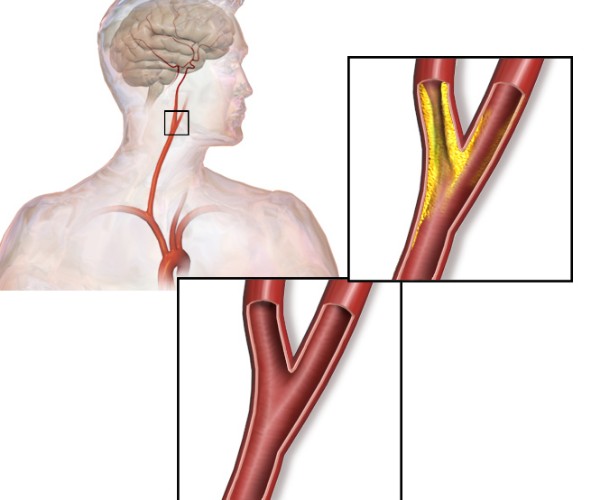
A stent un is small, mesh-like tube composed of inert material of various types (usually, metal, coated or uncoated with carbon) and impregnated or unimpregnated with specific pharmacological ingredients (medicated or unmedicated stent). Typically, a stent is applied to consolidate the result of reopening a cardiac vessel occluded (completely or partially) by a thrombus and/or atherosclerotic plaque as part of a hemodynamic procedure known as angioplasty.
In principle, any occluded artery can be treated with angioplasty and stent application, but usually the vessels undergoing this type of procedure are mainly the coronary arteries (the arteries that supply the heart muscle, supplying it with oxygen and nutrients).
Symptoms
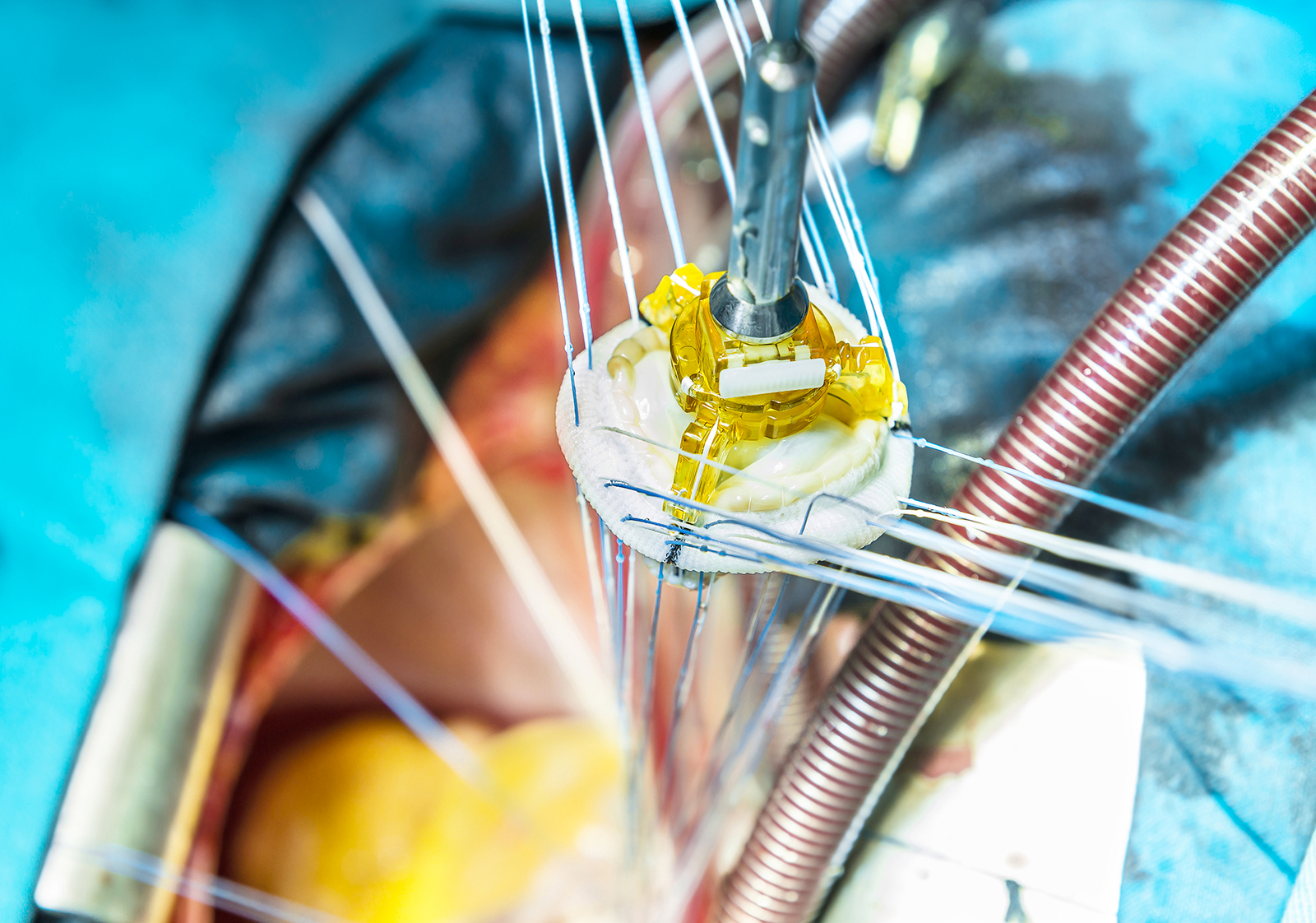
The application of a stent is done percutaneously by inserting the surgical catheter into a small incision made at the level of a navigable peripheral artery, usually at the level of the groin (femoral artery), elbow socket, or wrist, depending on the preferred route to the heart in the individual patient.
A balloon surrounded by the stent is placed at the end of the surgical catheter.
Once at the site of the artery to be treated, the balloon is allowed to expand, and the stent goes on to compress the atherosclerotic plaque against the vessel walls, increasing the caliber of the free lumen, again available for blood flow.
After compression of the plaque and placement of the stent, the balloon catheter is removed, retracing back through the vessels initially navigated.
If the applied stent is of the nonmedicated type, the only action exerted is mechanical (plaque compression), whereas if the retina is coated with drug-impregnated plastic material, there is an additional action directed at counteracting cell proliferation, inhibiting plaque regrowth, and thus more effectively preventing possible recurrence.
Stent placement with angioplasty is performed under local anesthesia (administered in the area of catheter insertion) and subjecting the patient only to mild sedation; general anesthesia is not necessary, and the patient remains awake throughout the procedure.
The entire procedure is performed under cardiac monitoring to catch any alteration in the heart’s contraction rhythm promptly.
One or more of the same or different stents may be applied during the same intervention session.
If the procedure is performed for preventive (planned) purposes, generally the required hospital stay is 24 hours, whereas if the angioplasty is performed in an emergency, in conjunction with a myocardial infarction, the length of hospitalization will vary depending on the type/severity of acute event that occurred and the patient’s overall response to treatment.
Diagnosis
Angioplasty with stent insertion can be performed as a preventive measure, after detecting a localized partial occlusion of the blood vessel during a cardiology checkup or immediately after a myocardial infarction, to quickly restore blood flow in the coronary arteries and contain damage to the heart.
The presence of the stent within the blood vessel keeps its walls spaced apart, greatly reducing the risk of new occlusions and, consequently, of severe acute cardiac events.
The application of stents for preventive purposes is generally recommended when the damage caused by atherosclerosis is already significant and drug therapy can no longer provide adequate protection from symptoms that may reduce quality of life (angina, chest pain, shortness of breath, weakness, palpitations, etc.) and, above all, from severe acute cardiovascular events (myocardial infarction).
If the critical atherosclerotic plaque is located at the bifurcation of two arteries or in another area where the stent cannot be applied, and when the vessels are seriously damaged by atherosclerosis in several places, it is usually preferable to proceed with the application of coronary bypass, corresponding to the replacement of the damaged section of blood vessel with a piece of healthy vessel, taken from another part of the body.
The choice of the type of surgery to be performed (stent angioplasty or cardiac surgery with by-pass) will be made on the basis of a careful assessment of the type of arterial problem present, the overall cardiologic status and clinical picture, the patient’s age, any copathologies, the feasibility of each of the two procedures, and the associated operative risks.
Among the lifestyles
After the application of one or more stents, patients feel better overall, being able to breathe without (or with less) wheezing and tolerating exercise more.
However, it should be remembered that the atherosclerosis that necessitated the need for angioplasty is a chronic condition that can affect all arteries and tends to worsen over time, even in the face of taking appropriate drug therapy.
After stent placement, therefore, it will be essential to take all prescribed medications regularly, undergo periodic cardiology checkups, and follow a healthy lifestyle and the common cardiovascular prevention rules recommended even for those who have never had cardiovascular problems.
That is, maintain a healthy diet (rich in fruits and vegetables, fish and legumes and low in saturated fat, salt and red meat), engage in moderate physical activity compatible with one’s potential, and avoid mental and physical stress, smoking and excess alcohol.
In the period following the application of one or more stents, moreover, the patient is at an increased risk of clot formation at the device and, consequently, of experiencing acute thromboembolic events.
To minimize this, it will, therefore, be essential to take anticoagulant/antiaggregant therapy for a variable period of time determined by the physician on a case-by-case basis, also depending on the type of stent applied (typically, one year).