All
antibiotics
should be used with caution, only when prescribed by a physician to treat a bacterial infection of some importance that could not heal on its own, and should be taken by carefully following the directions regarding dosage, timing, and mode of administration. The use of some antibiotics, however, requires more caution than others because the side effects that may result from their action in the body are particularly severe.
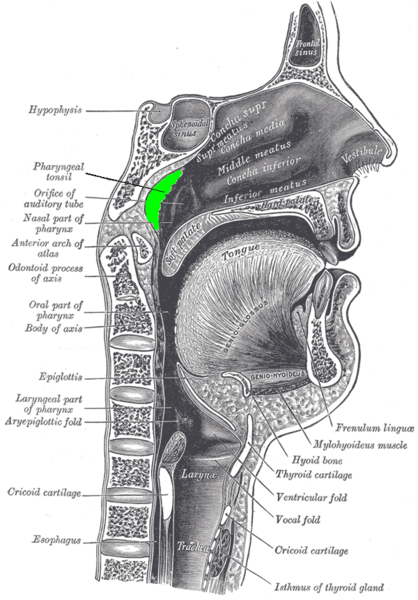
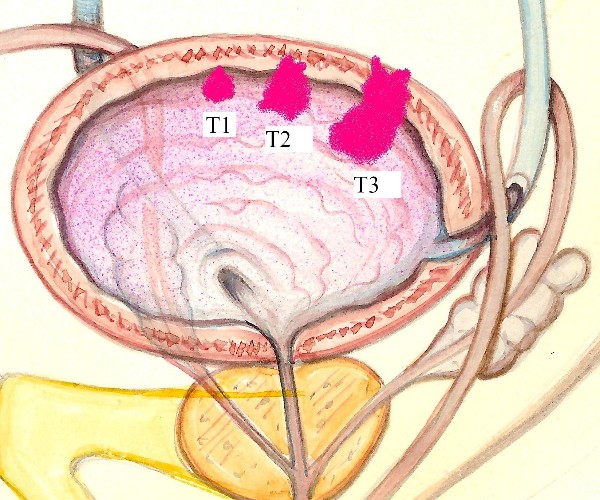
Among them are the fluoroquinolones: a class of broad-spectrum (i.e., effective against an extensive number of Gram+ and Gram- bacteria) antibiotics that have been used for more than 30 years for the treatment of serious and life-threatening bacterial infections, especially of the respiratory and urinary tracts, the gastrointestinal tract, and the bones.
In addition to the already known adverse events of these drugs, two reviews conducted by the European Medicine Agency(EMA) and the similar U.S. agency (FDA, Food and Drug Administration) during 2018 revealed additional significant critical issues that dictate that the use of systemically administered fluoroquinolones (i.e., by mouth, through injections, or by inhalation) should be limited exclusively to situations where no effective therapeutic alternatives are available to clear the body of infections so severe that they are life-threatening.
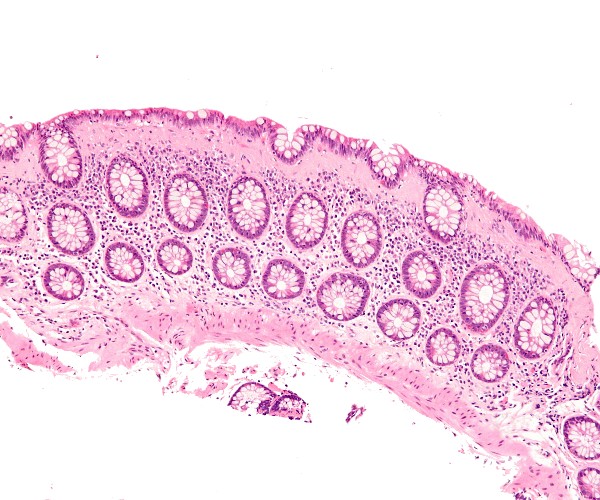
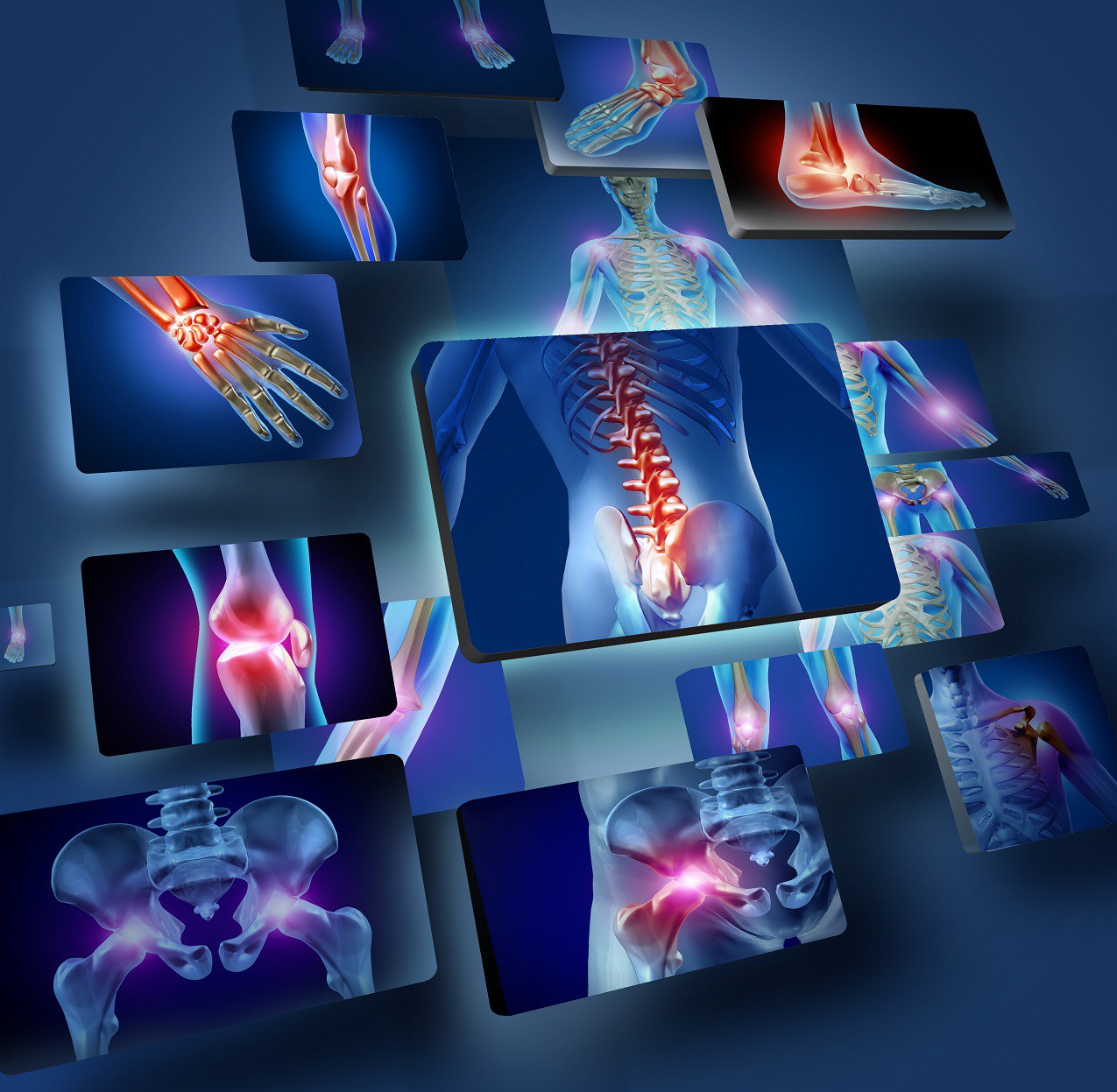
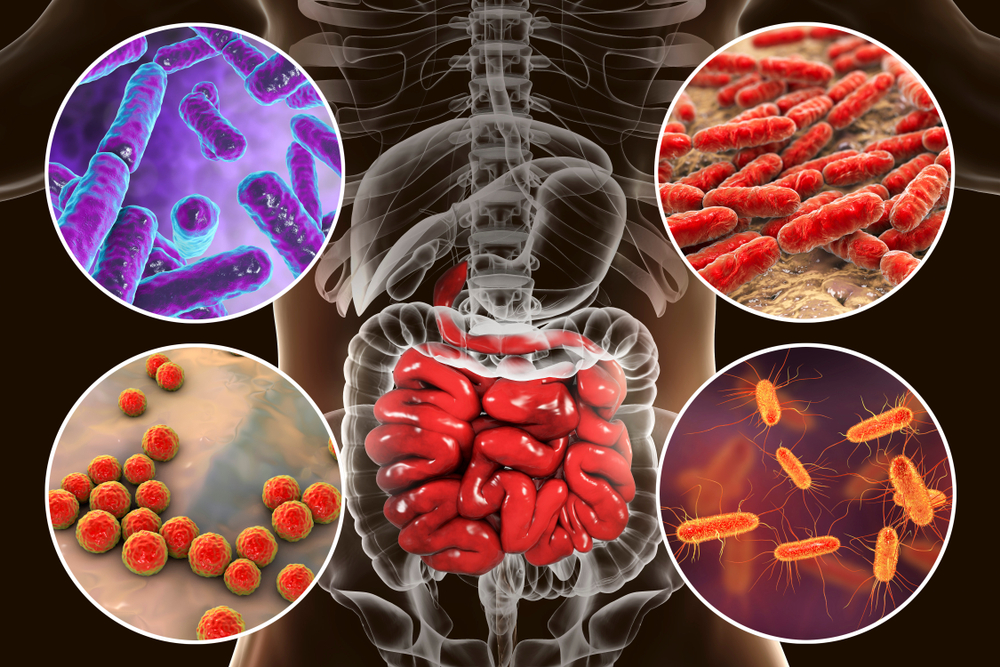
As early as November, the EMA had reported that taking systemic fluoroquinolones may be associated with Severe and disabling adverse events, long-lasting and potentially permanent, at the level of the muscles, bones, joints, and nervous system, in addition to those already known to affect the gastrointestinal system (risk of severe diarrhea, especially from Clostridium difficile) and cardiac (with contraindication for use in people with long QT syndrome and/or bradycardia, i.e., slow heartbeat).
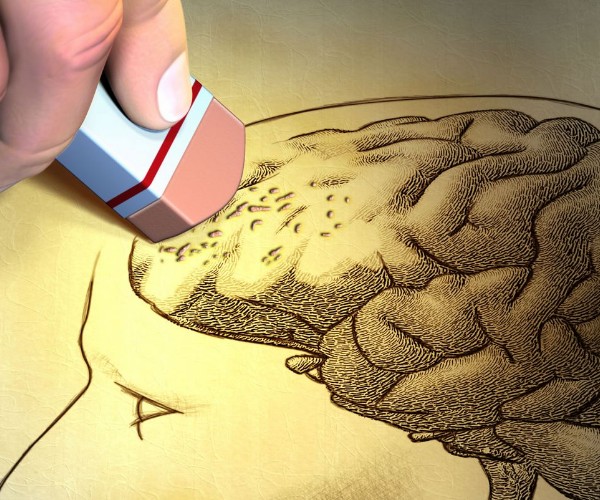
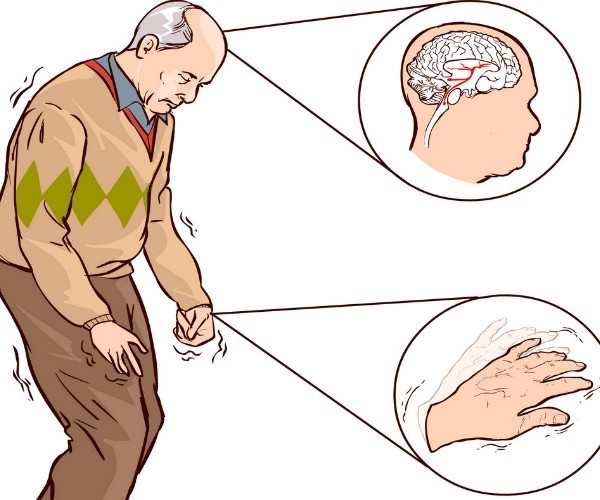
These serious side effects of commercially available fluoroquinolone antibiotics (ciprofloxacin, levofloxacin, lomefloxacin, moxifloxacin, norfloxacin, ofloxacin, pefloxacin, prulifloxacin, and rufloxacin) include inflammation and rupture of tendons (especially the Achilles tendon of the ankle), muscle pain or weakness and joint pain or swelling, difficulty in walking, neuropathy and paresthesias (feeling of pins and needles, burning, etc.), fatigue, depression, memory problems, impaired sleep, vision and hearing, impaired taste and smell.
The appearance of swelling and injury at the level of tendons can occur within two days of the start of treatment with a fluoroquinolone antibiotic or several months after its discontinuation, and it is this long interval between taking the therapy and the appearance of the side effect that for many years prevented physicians from understanding the actual correlation between the two events and, therefore, the significance of the risk associated with the use of these drugs.
The likelihood of occurrence of the mentioned adverse events is higher in people over 60 years old, in those who already have problems with Musculoskeletal or renal level or has received an organ transplant and in those who are also taking or have recently taken corticosteroid medication systemically (by mouth, injections, inhalation) or jointly (infiltrations) to treat other conditions.
But it is not over. Just before Christmas, the FDA added an additional and more alarming rationale for limiting the use of fluoroquinolones as much as possible. In fact, according to audits conducted by the U.S. agency, treatment with these antibiotics is also associated with an increased risk of dissection and rupture of the aorta: the body’s main artery that collects oxygenated blood exiting the heart and distributes it throughout the body.
At greatest risk of such events (which place the affected person in immediate life-threatening danger and therefore represent an absolute medical emergency) are especially the elderly and those who have or are at risk of developing aortic aneurysms, such as people suffering from atherosclerosis, high blood pressure, and/or certain predisposing genetic conditions such as Mafran syndrome and Ehlers-Danlos syndrome.
In all of the above cases, fluoroquinolones should not be used unless they represent the only class of drugs available to treat a life-threatening infection, and their eventual use should always be closely monitored by the physician, however.
All people on systemic fluoroquinolone antibiotic therapy should follow the doctor’s instructions, without spontaneously discontinuing treatment, and immediately report any onset of symptoms such as:
- Pain or inflammation in the Achilles tendon (or other tendons);
- Pain, burning, tingling, numbness, or weakness in the arms and legs or other parts of the body;
- Severe pain behind the sternum or in the upper back (similar to that of a heart attack), radiating to the neck, shoulders, and jaw;
- Severe abdominal or lower back pain radiating to the legs.
Source
- Fluoroquinolone Antibiotics: Safety Communication – Increased Risk of Ruptures or Tears in the Aorta Blood Vessel in Certain Patients(https://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm628960.htm)
- Important Information Note on Medicines Containing Fluoroquinolones(http://www.aifa.gov.it/content/nota-informativa-importante-su-medicinali-contenenti-fluorochinoloni-23102018)
- Disabling and potentially permanent side effects have led to discontinuation or restrictions in the use of quinolone and fluoroquinolone antibiotics. EMA/795349/2018 (https://www.ema.europa.eu/en/news/disabling-potentially-permanent-side-effects-lead-suspension-restrictions-quinolone-fluoroquinolone)